How Your Sleeping Position Could Be Quietly Sabotaging Your Herniated Disc Recovery?
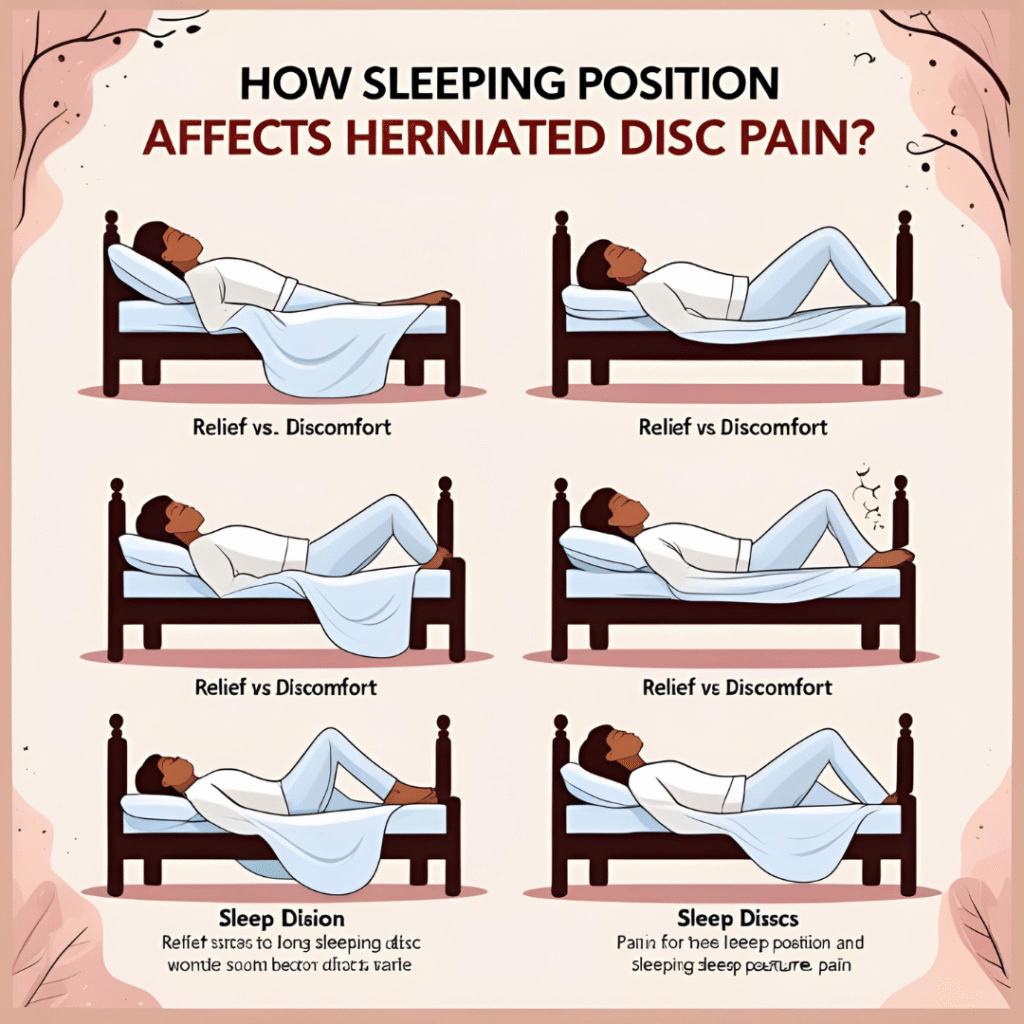
How Sleeping Position Affects Herniated Disc Pain? If you’ve ever been woken up at 2 a.m. by a lightning bolt of pain shooting from your back to your toes, you already know: nighttime is when a herniated disc likes to remind you who’s boss.
The good news? A few simple tweaks to how you lie in bed can turn those midnight torture sessions into genuine, healing rest. Below, we’ll unpack the science behind why position matters, walk through the best options for each disc location, and share quick hacks you can try tonight—no fancy hospital bed required.
Why lying down can hurt more than standing up
During the day, gravity keeps your vertebrae stacked like a neat pile of coins, discs happily sandwiched in between. The moment you lie flat, especially on a soft mattress, the natural “S” curve of your spine flattens. The movement increases stress on the injured disc, making it protrude slightly more. Your goal in choosing a sleeping posture is to recreate the curves your spine loves while you’re upright, so the disc can stop yelling at the nerves and start healing.
Lower-back herniations: Side-lie like a pro
About 90% of disc injuries occur in the lumbar spine. If you’re among them, the classic side-lying position—with a pillow between your knees—can help. This trick keeps your pelvis level and prevents the top leg from tugging your spine into a twist.
Prefer a little more curl? Roll gently into a loose fetal position—knees toward chest, shoulders slightly forward. This increases the gaps between the vertebrae, in result giving the disc room to rehydrate and relieve the pressure.
Just remember to swap sides every couple of nights, or you’ll wake up with new hip or shoulder aches from asymmetry.
Neck-level trouble: Keep it neutral
Your pillow can be a game changer for you. On your back, choose a thin pillow (about two to three inches thick) so your head stays in line with your spine, not pushed forward like a turtle. Keep in mind that Side-sleepers always need a thicker pillow and size of that pillow should be approximately 4 to 6’’—to fill the gap between ear and shoulder. Too high or too low, and the neck flexes or extends, clamping down on already-irritated nerves.
Upper-back (thoracic) herniations: Recline and relax
Thoracic disc pain is rarer but just as irritating. Semi-reclined position sleep is One of the easiest way to fix. You don’t need a La-Z-Boy; a wedge pillow or an adjustable bed base can create a gentle 30-45° angle between thighs and trunk. This angle unloads weight from the mid-spine and lets the paraspinal muscles finally clock out for the night.
Stomach sleeping: Proceed with caution (and props)
Most experts wave red flags at stomach sleeping because it exaggerates the lumbar arch and forces the neck into rotation. Still, if you can’t fall asleep any other way, place a thin pillow under your pelvis and lower abdomen to keep the spine closer to neutral. Skip the head pillow or use a very flat one to avoid cranking your neck backward.
The mattress conversation
All the perfect pillows in the world won’t save you if you’re sinking into a 15-year-old marshmallow. A medium-firm mattress—think supportive but not concrete—keeps your spine from bowing downward. Can’t swing a new bed? A two-inch memory-foam topper on top of the existing mattress buys you time and comfort.
Micro-movements: Your secret weapon
Staying frozen in one position all night actually increases stiffness. Before you drift off, set a silent intention to shift slightly every hour or so. Even rolling from left-side fetal to right-side fetal counts. When you wake up, hug your knees to your chest for 30 seconds before standing; it primes the discs for the day’s load and reduces that infamous “morning concrete back.”
Quick checklist for tonight
- Identify your disc level: lower, neck, or mid-back.
- The best position for thoracic disc pain would be reclining, as it helps offload pressure on the mid-spine and reduces irritation.
- Between your knees, under your thighs, or supporting your neck—experiment with different pillows to find the perfect setup.
- If you’re a stomach sleeper, add the pelvic pillow safety net.
- Test-drive the setup for 10 minutes before lights-out; small adjustments now save 3 a.m. frustration.
When to call in the pros
If pain still disrupts your sleep after two weeks of adjusting positions—or if you notice worsening leg weakness or numbness—it’s time to consult a spine specialist. Night pain that responds to conservative changes, though, usually calms down within days once your sleeping posture stops shouting at the injured disc.
Bottom line:
You can’t rush the biology of disc healing, but you can give it the best possible environment to do its job. Align the spine, unload the pressure, and let your pillow do the heavy lifting—while you finally get some actual rest.